Endocrine
System |
Hypophysis
• It has a dense connective tissue capsule that comes
from the dura mater that sends septa into the organ.
• It has three portions: the anterior portion(or adenohypophysis),
the posterior portion (or neurohypophysis) and the intermediate
portion.
• The adenohypophysis originates from the epithelium that
evaginates and stands out from the hard palate (Rathke Pouch),
migrating towards the neural tube.
• The neurohypophysis is an evagination of the floor of
the diencephalus
• It is a gland that produces numerous important hormones
and therefore is acknowledged as the master-gland of the nervous
system.
• Responsible for regulating the activity of other glands
and various other functions of the organism such as growth and
the secretion of milk from the mammary glands.
•
It is richly vascularized as all endocrine glands are since
the hormones it produces are released into the blood vessels.
Constituents:
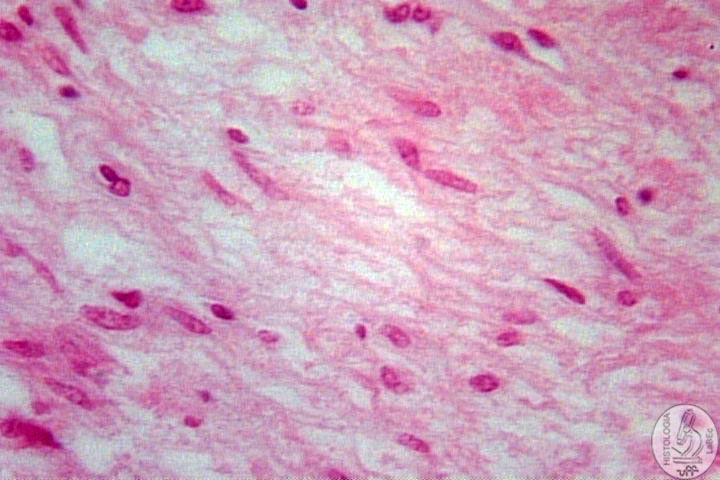
Neurohypophysis
• It
connects itself to the hypothalamus through the infundibulum.
• The hormones are produced in the cell body of the neurons
in the hypothalamus and these hormones are then transported
through the axons of the neurons towards the neurohypophysis
that releases these hormones when stimulated.
• The
hormones that are secreted through the posterior hypophysis
are: Oxytocin and ADH.
Oxytocin
• It comes from the paraventricular nucleus of the hypothalamus.
• It acts on the uterus helping it contract during labor
and in mammary terms it facilitates the secretion of milk
Antidiuretic
Hormone (ADH, Vasopressin or AVP-Arginine Vasopressin)
• It comes from the supraoptic nucleus of the hypothalamus
• It regulates the contraction of blood vessels, regulating
the pressure and antidiuretic action on the kidney tubules
Amyelinic
Axons
• Fibrillary extensions of the hypothalamic neurons, where
deposits of neurosecretion can be observed in its extremities
(Herring corpuscles)
• Presence of Fenestrated capillaries
|
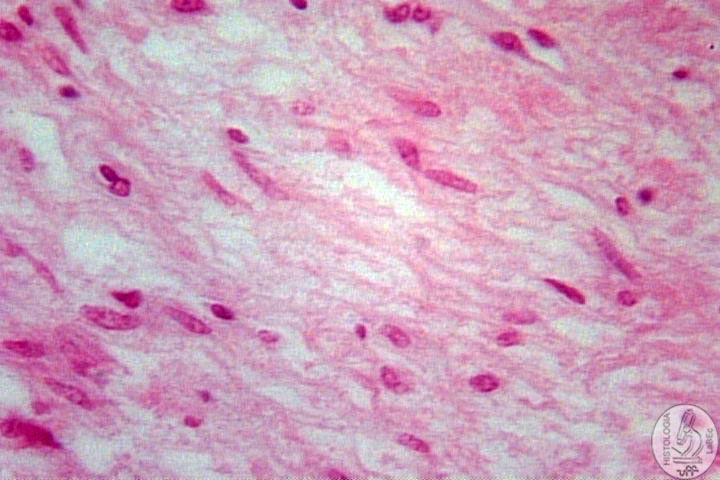 |
Pituicytes
• Constituent cells of the neurohypophyseal parenchyma
• It has an irregular shape with countless extensions. |
|
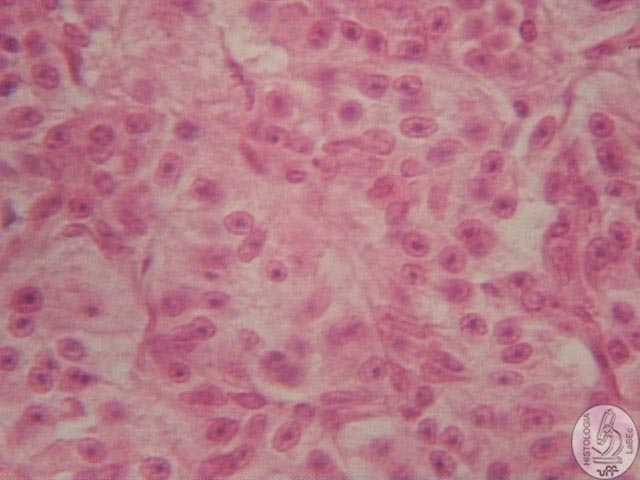
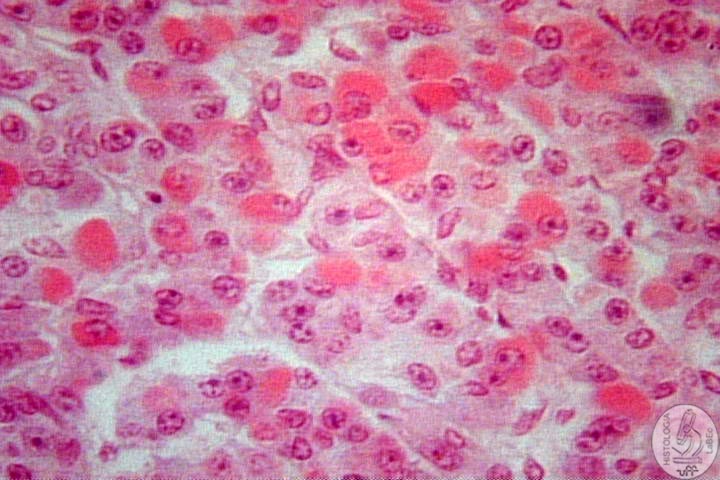
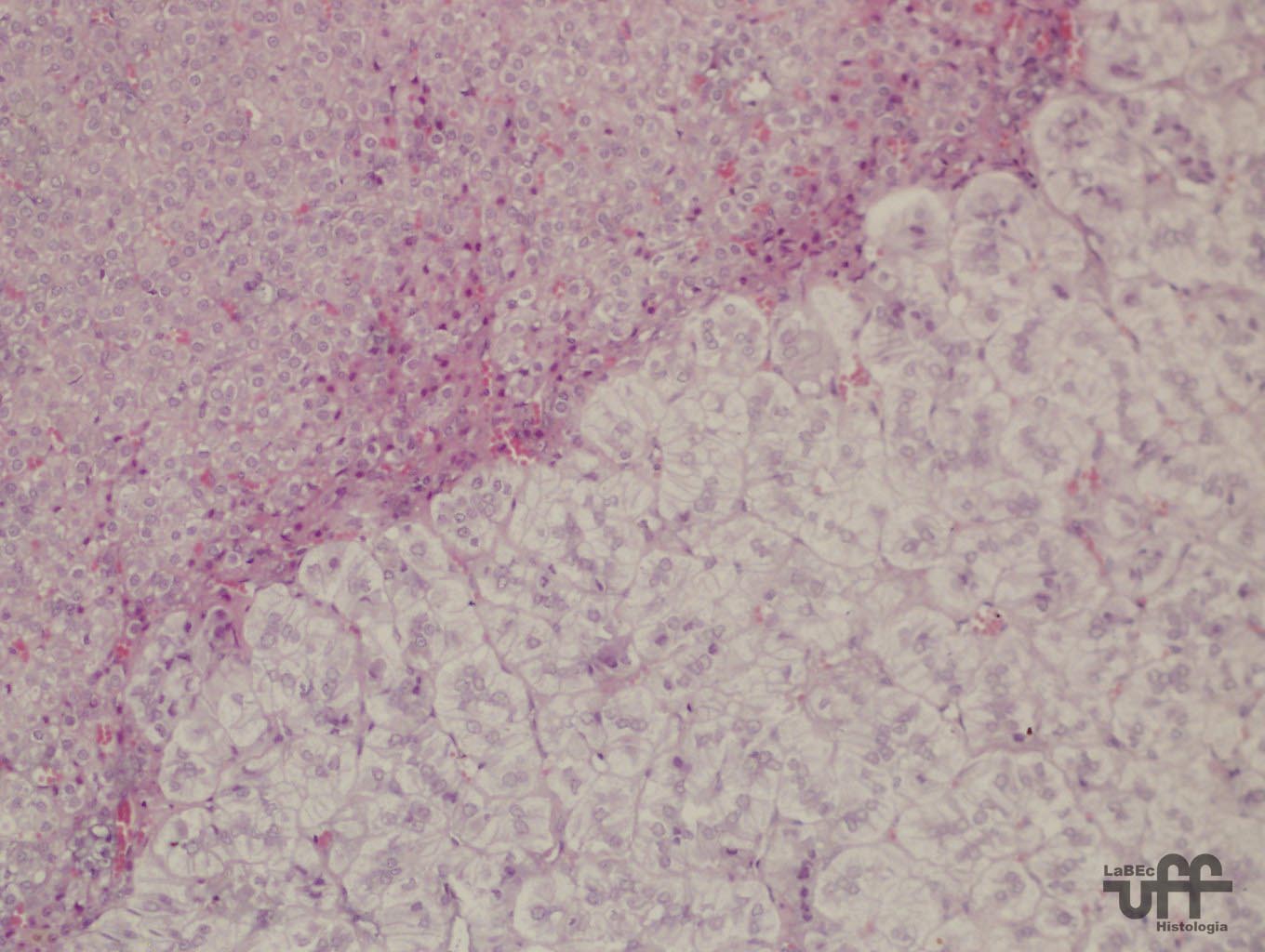
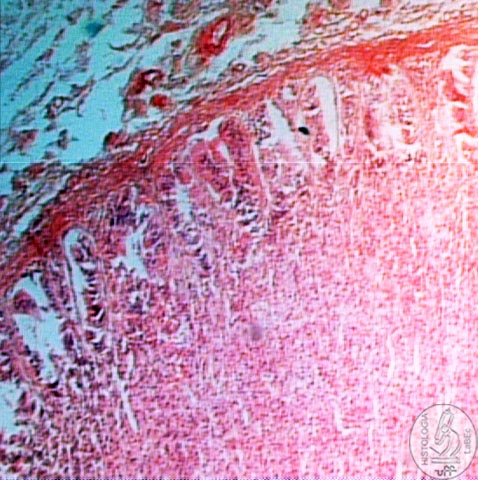
Adenohypophysis
• Through the vascular connection of the adenohypophysis
with the hypothalamus, the hypothalamus integrates central and
peripheral stimulatory and inhibitory signals to the five types
of phenotypically distinct hypophysis cells.
• Histologically, we observe 3 cell types, differed by staining,
which are:
- Chromophobic cells (cytoplasm does not have an affinity for
stains; only the nuclei stained with hematoxylin are observed)
- Chromophilic cells
A) Acidophilic (cytoplasm stained by eosin)
B) Basophilic (cytoplasm stained by hematoxylin)
|
| 
|
Adenohypophysis |
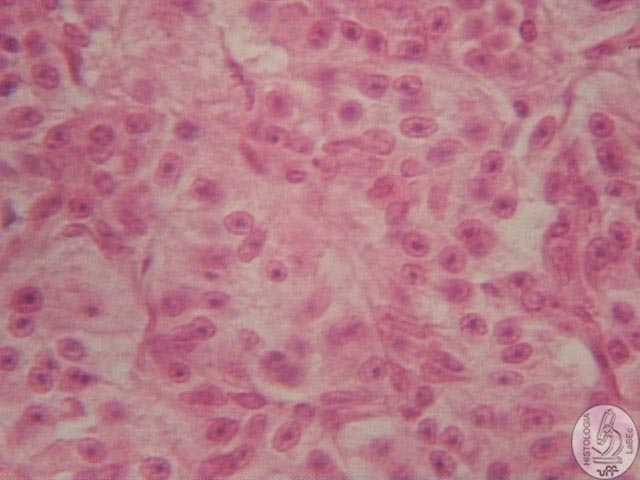 |
Chromophobic
Cells |
 |
Chromophilic
Cells |
|
Chromophilic
Cells |
| Adenohypophysis |
Hypothalamus |
Stains
(Type) |
Cell
Type |
| Growth
H. (GH) |
GHRH(
Growth hormone releasing hormone) |
Acidophilic |
Somatotroph |
| Prolactin |
Secretion
inhibited by DA (dopamine) |
Acidophilic |
Lactotroph |
| Follicle
Stimulating H. (FSH) |
GnRH(Gonadotropin
releasing hormone) |
Basophilic
|
Gonadotroph |
| Luteinizing
H. (LH) |
GnRH(Gonadotropin
releasing hormone) |
Basophilic
|
Gonadotroph |
| Thyroid
Stimulating H. |
TRH(
Tireotropin releasing hormone) |
Basophilic
|
Tireotroph |
| Adrenocorticotrophic
H. |
CRH
(Corticotropin Releasing Hormone) |
Basophilic
|
Corticotroph |
| Endorphins |
- |
- |
- |
|
| Intermediate
Portion
• Stimulates the melanocytes (MSH): regulates the distribution
of pigments.
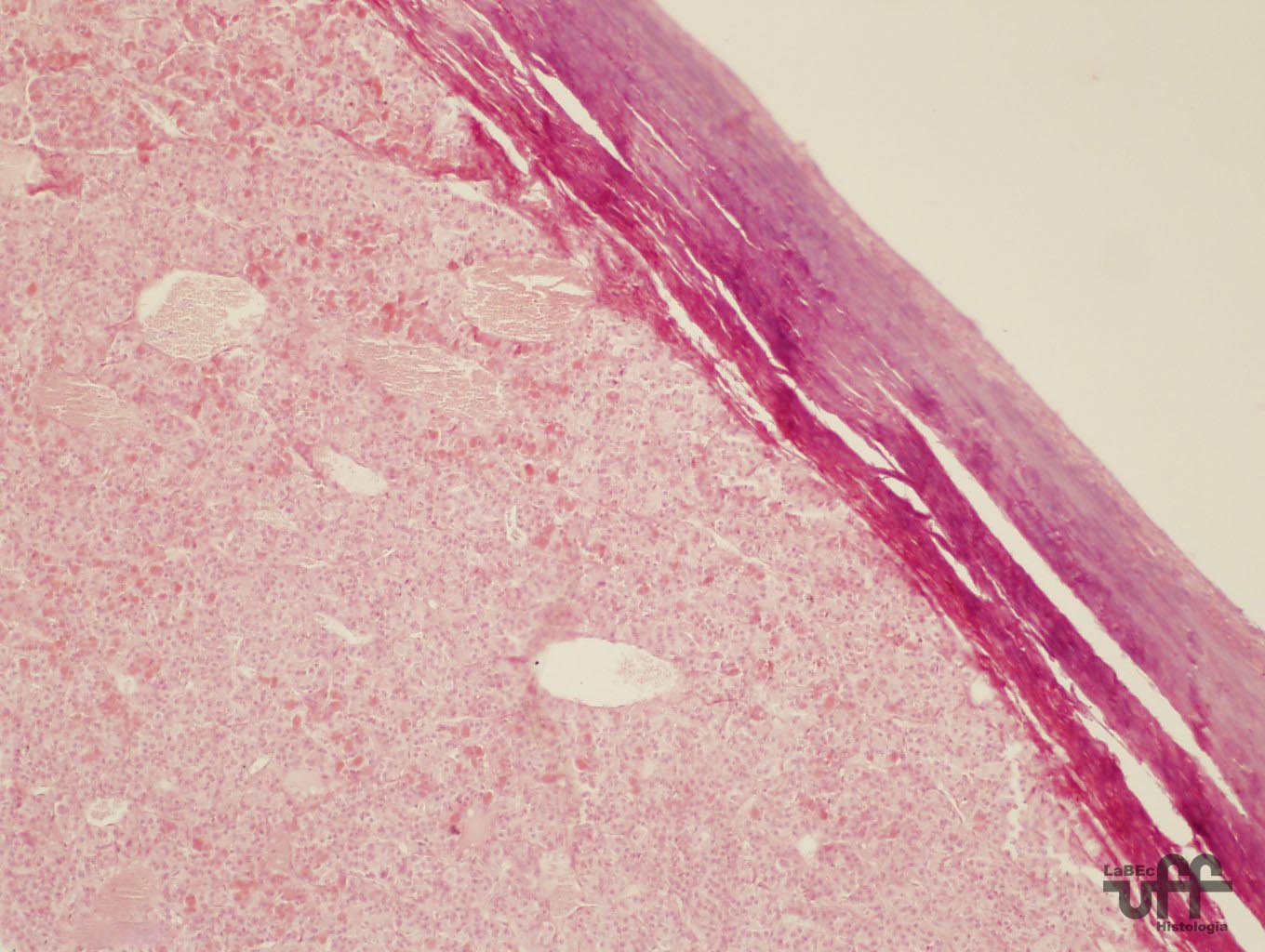
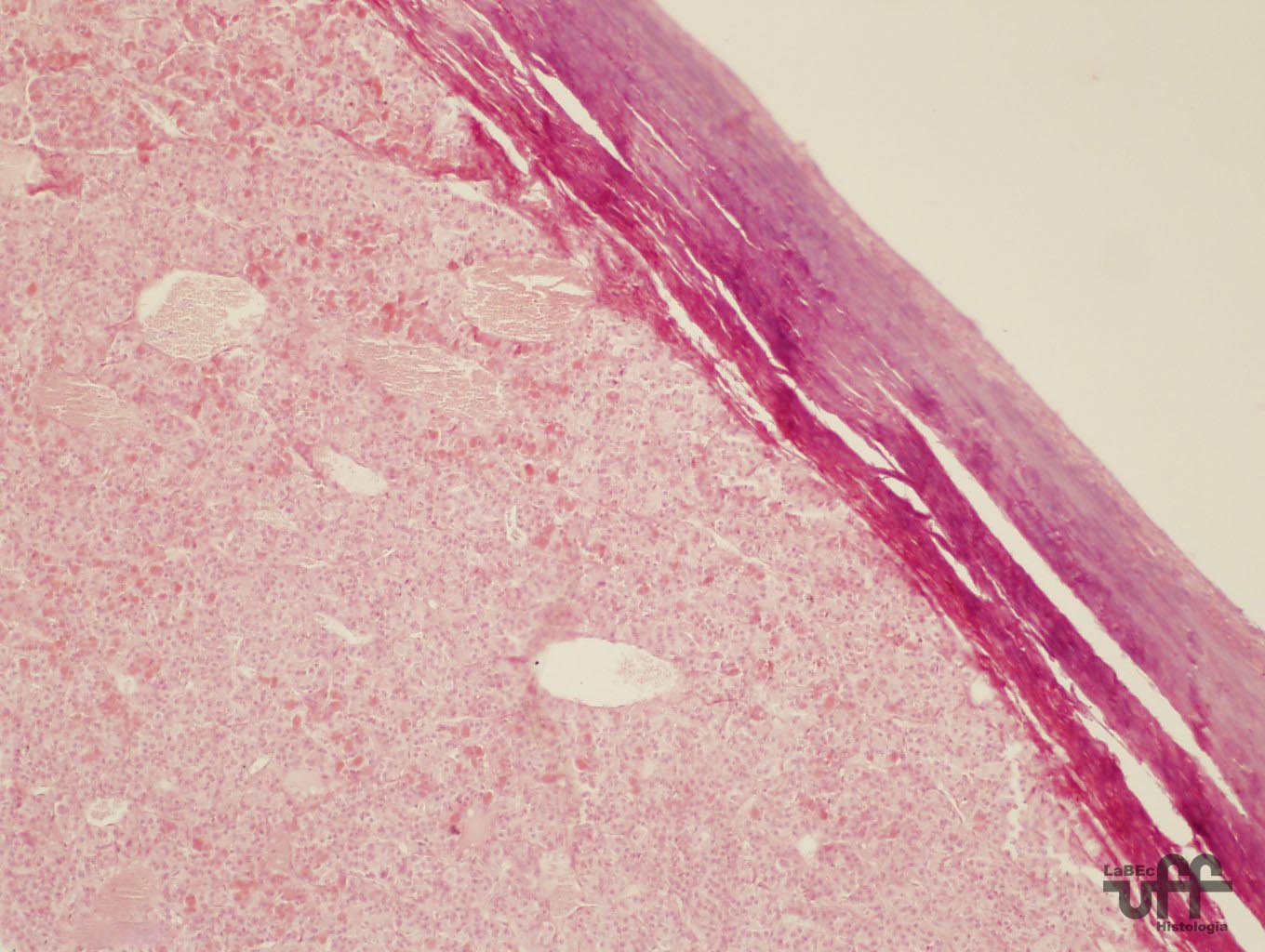
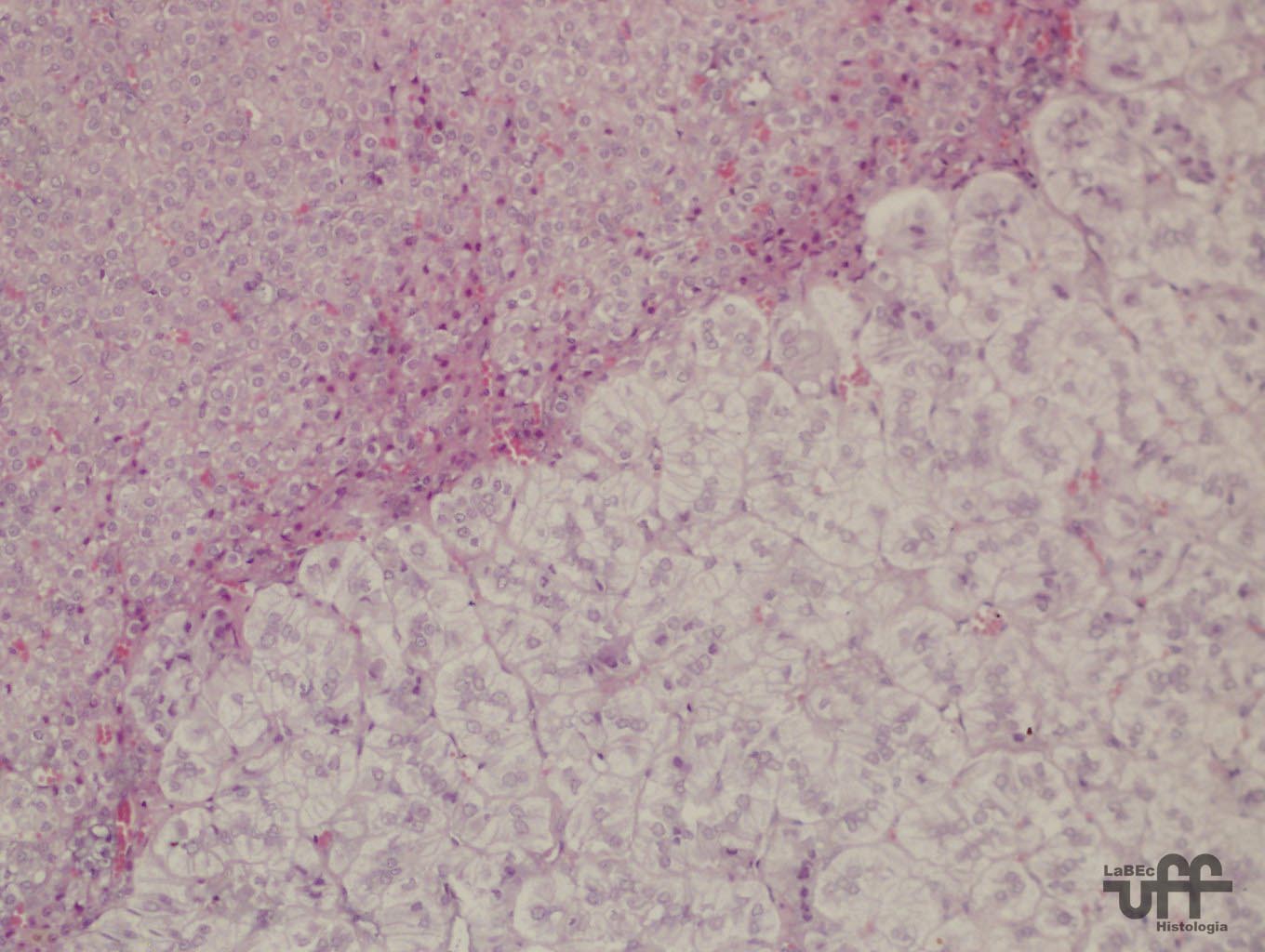
| Adrenal
Glands
• They are endocrine glands covered by a fibrous,
innerved and vascularized connective capsule.
• Its main function is to stimulate the conversion
of proteins and fat into glucoses at the same time it reduces
the capture of glucoses by cells, therefore increasing the
use of fat, and consists on the synthesis and release of
corticosteroid hormones and cathecolamines, such as cortisol
and adrenaline.
• Histologically,
it is divided into a cortex and medulla. |
|
|
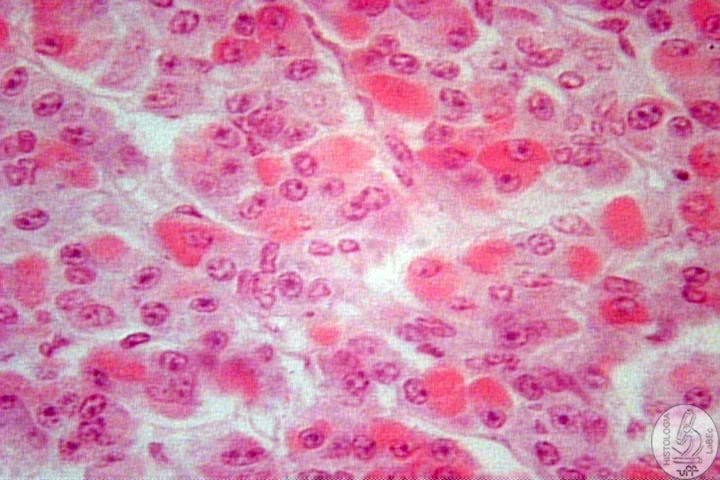
Cortex
• Outer part of the gland with a yellowish color due
to the great amount of cholesterol there.
• It has an embryonic origin in the mesodermis. It
subdivides itself into three regions due to their different
histological aspects. |
Glomerular
Zone
• The outermost zone, presents cell cords disposed
in arches.
• There
are juxta-vascularly disposed columnar cells in such a way
that resembles a glomerulus
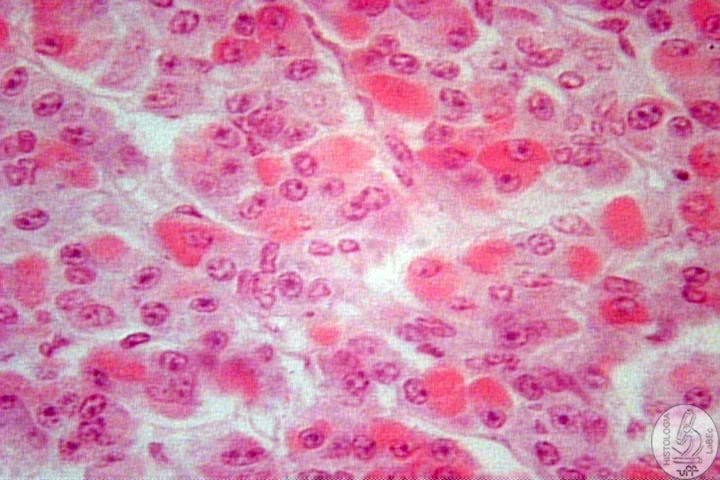
Fasciculate
Zone
• It is of intermediate location. The cells arrange
themselves parallel to each other and perpendicular to the
capsule of the gland
• The
cells are cuboidal and arrange themselves axially and juxta-vascularly
• The cytoplasm of its cells contains numerous vacuoles
giving them a spongy aspect and therefore are called spongiocytes.
Reticulated
Zone
• The innermost zone, it presents cords of cells arranged
in a net-like way
• The cells are polyhedral and arrange themselves
in a way that resembles a juxtavascular reticulum
|
-
Glomerular Zone: synthesizes mineralocorticoids
(aldosterone)
- Fasciculate and Reticulated Zone: secrete
glucocorticoids, of which the most important is cortisol.
Also secrete sexual steroids such as testosterone.
|
| 
|
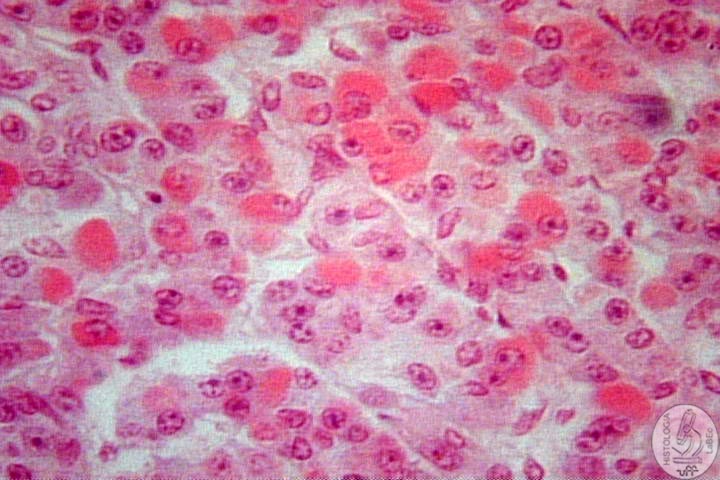
Medulla
• Inner part; derives from the neural crest. Its secreting
cells are polyhedral and organized into a network.
• There are two types of cells: Chromaffin cells and
Ganglionary cells that neighbor the capillary network.
• Synthesis and release of neuromediators, specially
adrenaline and noradrenaline. |
| >
The Cortex is essential to life, the Medulla is not. |
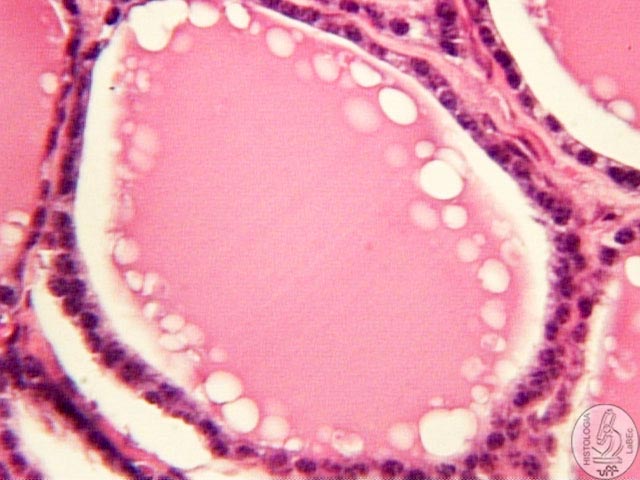
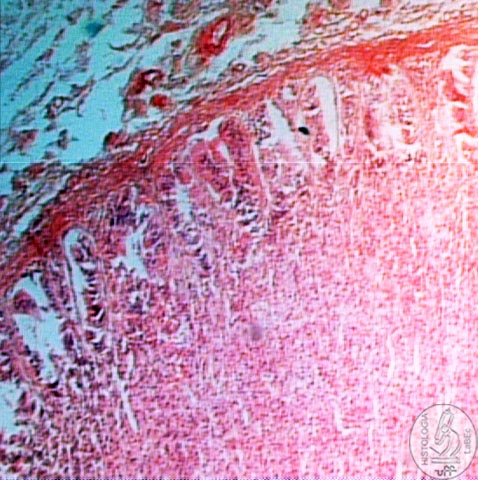
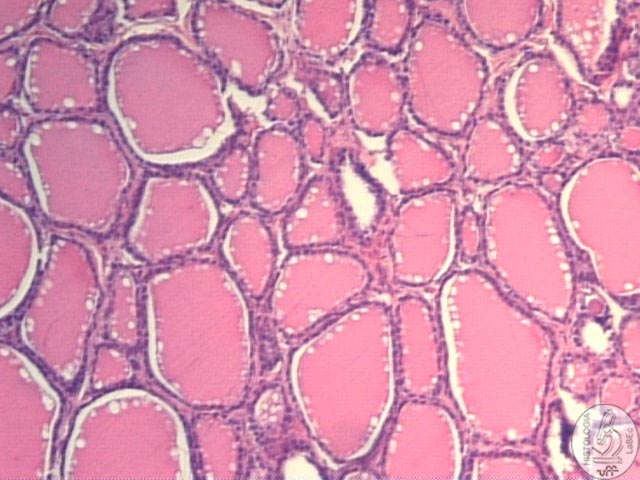
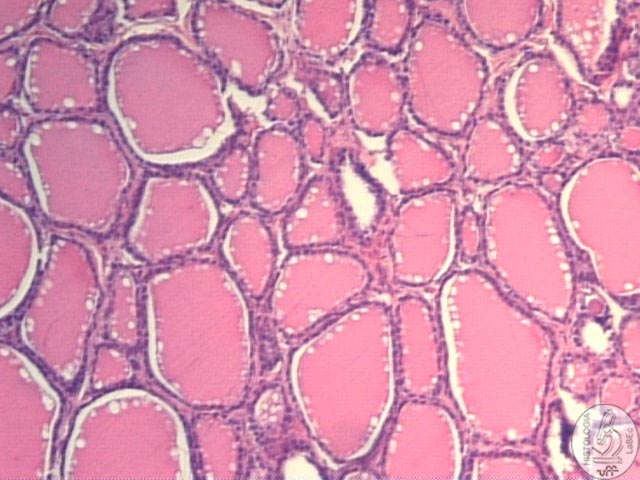
Thyroid
• It is a endocrine gland, covered by a fibrous connective
tissue capsule
• It has different shapes depending on the animal species
and is formed by two lobes united by an isthmus.
• The lobes are subdivided into lobules.
• The lobules are formed by vesicles or follicles lined
by simple cuboidal epithelium.
• Inside the vesicles we find the secreting material stored
in the form of colloid.
• The lining cells of the vesicles are called follicular
cells.
• Between the follicles, in the interstice, are the C (clear)
or parafollicular cells that produce calcitonin.
• The follicles are limited by a simple cuboidal epithelium
of follicular cells. These cells secrete into the follicle the
hormones and other substances that form the gelatin-like colloid
inside it.
• The colloid stores the thyroid hormone that is absorbed
once again by the follicular cells and released into the bloodstream.
|
|
Thyroid
Follicles |
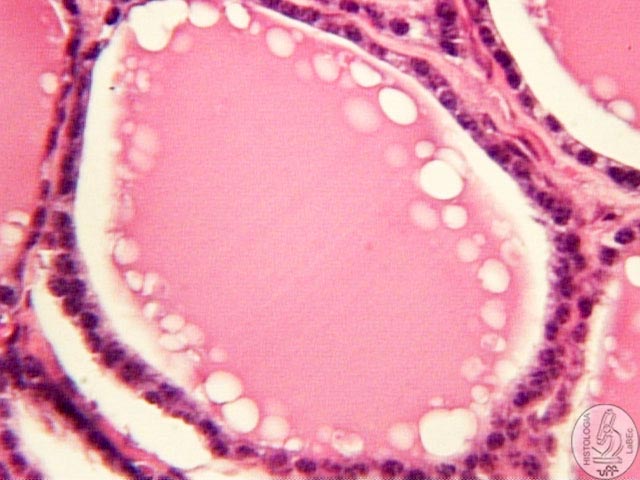 |
Follicular
Cells |
Functions
• The main function is to produce and store the thyroid hormones,
T3(tri-iodothyronine) and T4 (thyroxine);
• The production of these hormones occurs after the stimulation
of the cells by the hypophyseal hormone TSH
• The thyroid hormones T3 and T4 stimulate the cellular metabolism
by stimulating the mitochondria.
• The C cells produce calcitonin, a hormone that leads to
the reduction in the level of calcium in the blood(stimulating bone
formation)
• The thyroid is the only endocrine gland that stores its
secreting product. |
Parathyroid
• They are endocrine glands covered by a thin connective
tissue capsule of which thin septa emanate and penetrate the gland.
• It is not a lobulated gland
• The cells are densely grouped, in contrast to the follicular
structure in the thyroid.
• There are two kinds of cells, the main and the oxyphilic
cells, supported by a matrix of reticular and adipose connective
tissue.
• The main cells (eosinophilic) are smaller and secrete
the parathyroid hormone(PTH)
• The oxyphilic cells are larger and more basophilic and
have no known function.
Parathryoid
Hormone
• Stimulates the osteolytic activities of osteoclasts
• Increases the renal absorption of calcium
• Increases the absorption of vitamin D
• Increases the intestinal absorption of calcium
• All
this can be translated into a rapid and sustained increase in
the amount of calcium in the blood.
• It also influences the concentration of phosphate in the
blood, increasing the renal excretion of this ion by diminishing
its absorption in the renal tubules. |
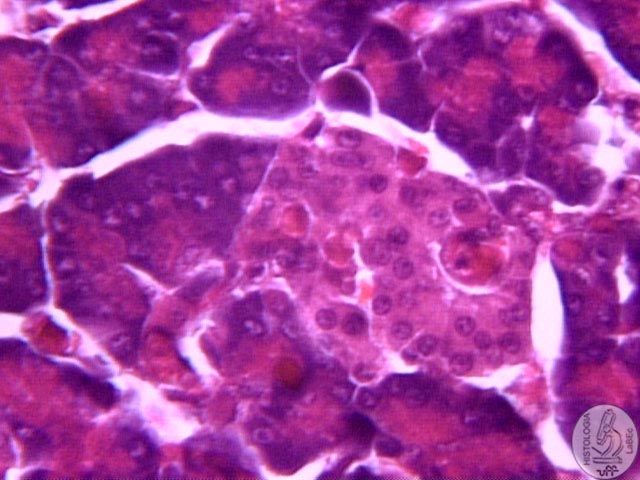
Endocrine
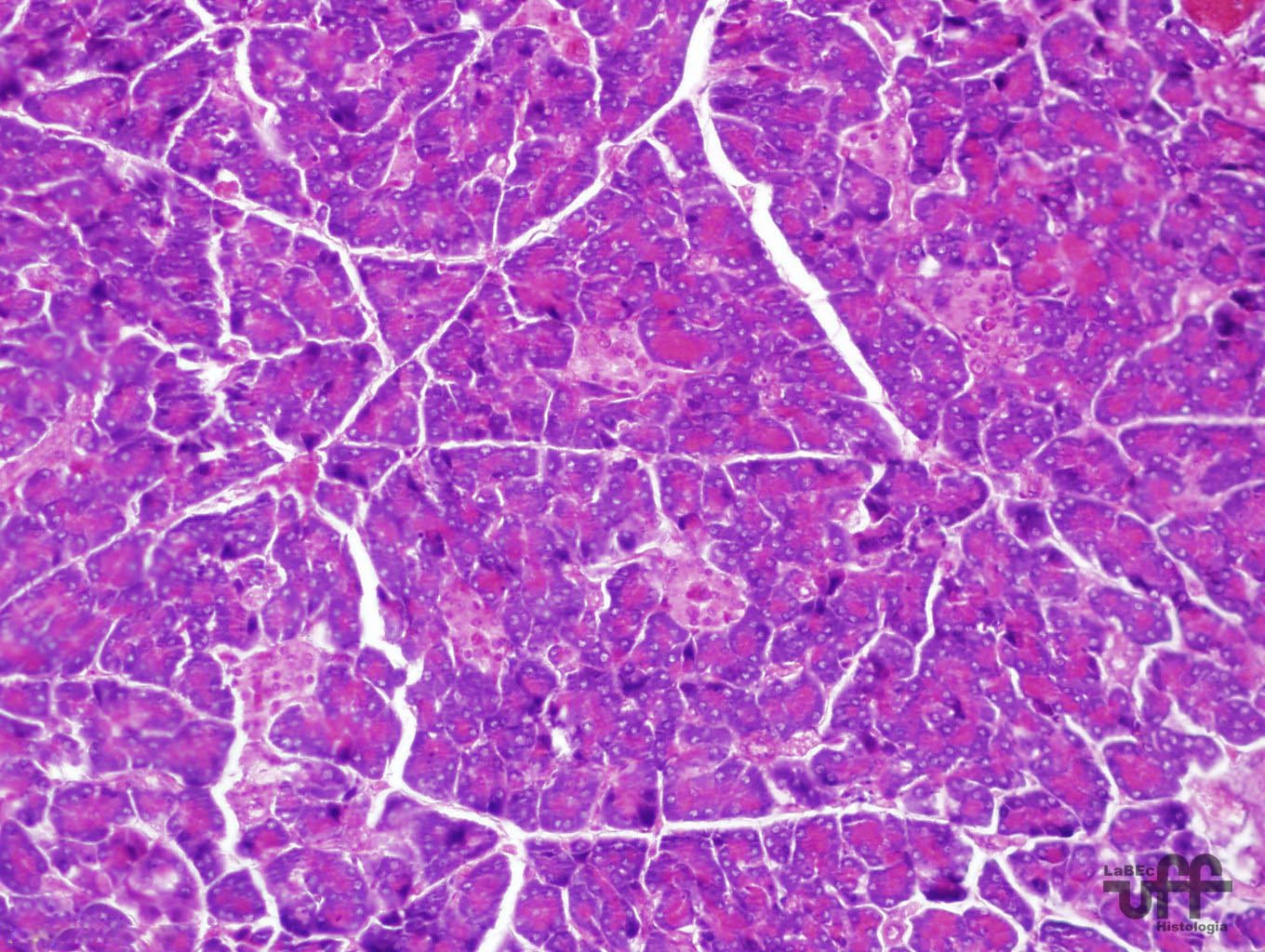
Pancreas
• Composed of agglomerations of special cells called Langerhans
islets
• There are 4 types of cells in the Langerhans islets. They
are relatively difficult to distinguish by average staining techniques
, but they can be classified according to their secretions:
|
Name
of Cells |
Product |
%
of Cells in the Islet |
Function |
| Beta
Cells |
Insulin
and Amylin |
50-80% |
Reduces
the level of sugar in the blood |
| Alpha
Cells |
Glucagon |
15-20% |
Increases
the level of sugar in the blood |
| Delta
Cells |
Somatostatin |
3-10% |
Inhibits
the endocrine pancreas |
| PP
Cells |
Pancreatic
Polypeptide |
1% |
Inhibits
the exocrine pancreas |
|
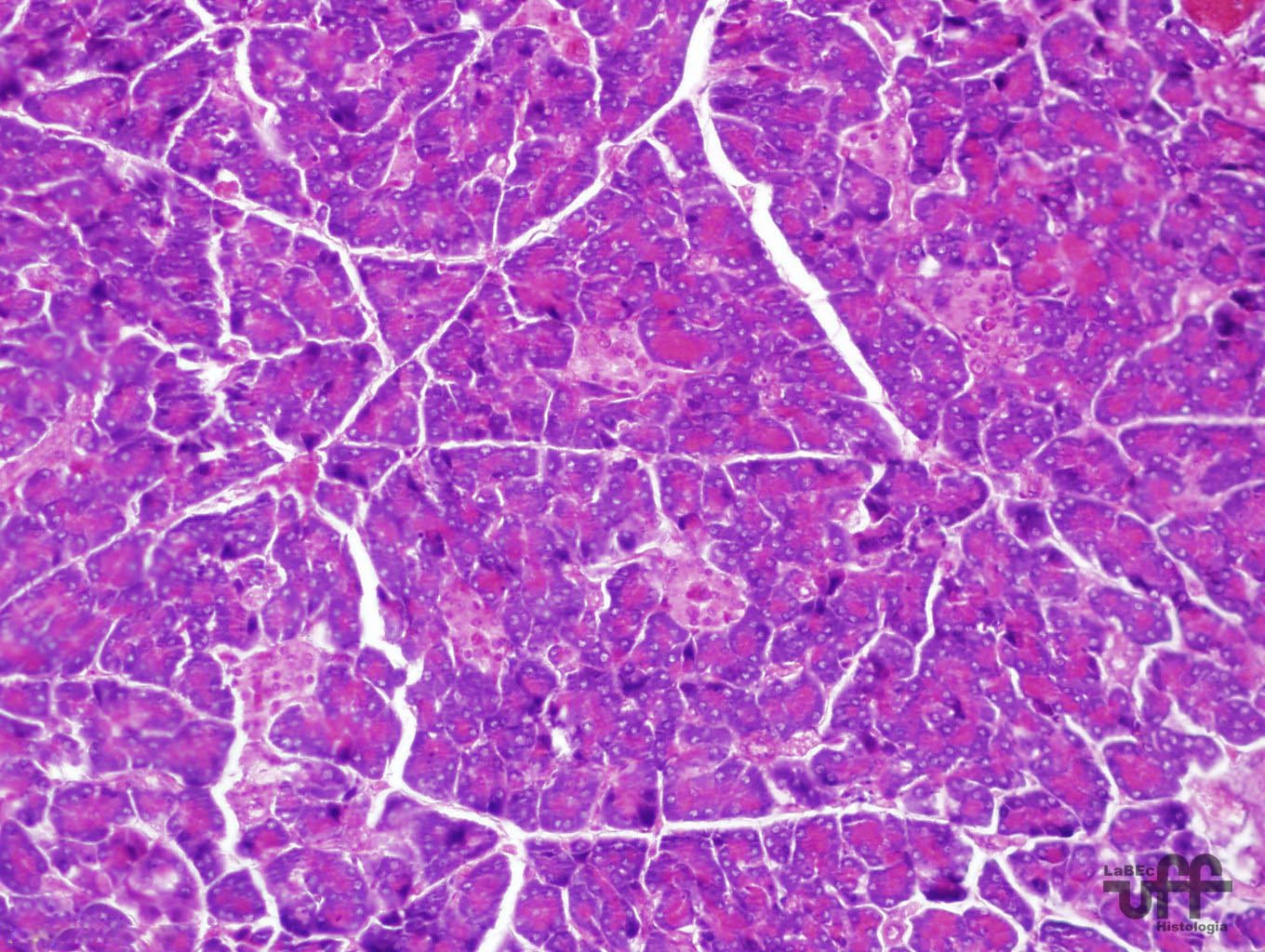 |
Pancreas |
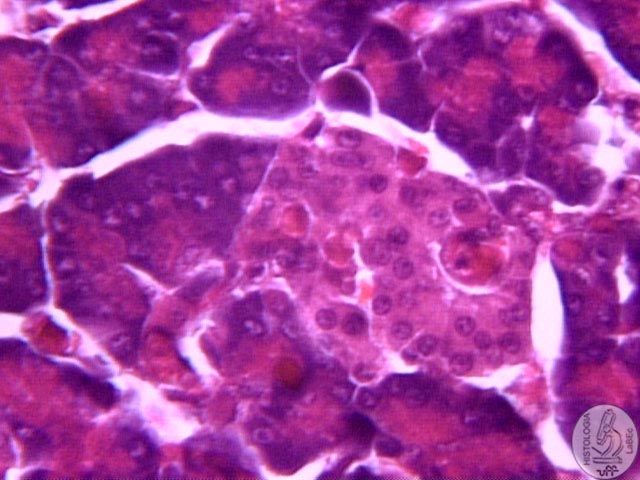
|
Langerhans
Islets |